By Richard E. Scott
Information and communications technology has revolutionized the types of partnership possible in research and care. Richard E. Scott Director of the Office of Global e-Health Strategy at the University of Calgary, advises on making wise investments and eliminating barriers to making full use of new technologies. —Report from a presentation at the 2012 conference of the MUHC-ISAI
Global e-health does not yet exist. We have some building blocks and we have some ideas about how it could be used to bring health benefits, but it is important that we proceed intelligently and cautiously because the potential for wasted effort and money is significant.
e-Health, however, does exist and is primarily comprised of four areas:
- Telehealth involves interaction between a patient and a clinician, or between clinicians, whether for consults in remote areas, home e-health or other.
- Health Informatics describes some kind of data collection and storage, conversion of that data into knowledge, and dissemination of that knowledge to users. Electronic health or medical records, personal health records, surveillance systems and decision-support systems fall into this category.
- e-Learning is the application of telehealth and health informatics to the education and continuing education of health professionals.
- e-Commerce includes the tools used to pay for health services.
The benefits of e-health
e-Health can work in many ways to level the playing field between different regions in access to quality health care. It does so by eliminating distance, whether between buildings on a hospital site, between regions in a province or country, or between different parts of the world. It also reduces the impact of time as it makes both synchronous and asynchronous communication possible. It increases access to information, education and services, while supporting standardizing processes to improve the consistency and quality of care, such as clinical practice guidelines.
e-Health could, it is felt, contribute to increasing the equity of health care across the globe. At present, the countries with the lowest burden of disease have the largest healthcare workforce, and countries with the highest burden of disease have the smallest healthcare workforce. e-Health’s potential to improve equity has been recognized by international organizations and leaders in the developing world. However, there are a number of important factors to consider in rolling out e-health programs.
Reality checks
How do people connect?
The places in the world that could most benefit from global e-health are found in South Asia, South East Asia, Sub-Saharan Africa and Latin America. The first question then is how are people connecting in these places. In Canada, we are looking to the Internet as the principal means of providing e-health services, and even here, our healthcare institutions are struggling to create the broadband width needed to make connections fast and reliable.
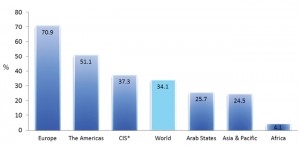
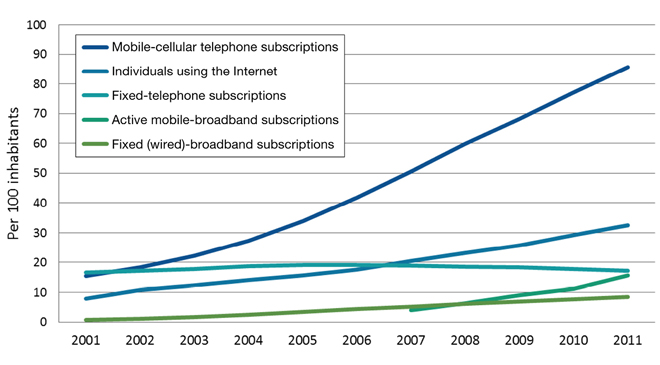
Figure 1 shows the percentage of households with Internet access by region, and it is evident that the places with priority needs are the least connected. Figure 2 provides a global picture of the information and communication technologies (ICTs) that are penetrating the world market most thoroughly, and mobile cellular telephones have an obvious, important and growing lead. In developing countries, the monthly cost of a mobile cellular telephone subscription is about $5 in purchasing power parity (PPP). The cost of a fixed broadband network subscription is about $200 in PPP. In Africa, 53 out of every 100 inhabitants have a mobile cellular subscription; less than 5% of households have Internet access.
Determining the readiness for e-health in a particular location is a key preliminary step, and there are tools available to help project leaders do that. These are not used often enough.
Who needs to be connected?
We are gradually moving beyond a paternalistic view of developed and developing nations, but there are still a great number of countries that lack the capacity to build their own capacity in health care. e-Learning can play an important role in supporting their efforts, and the connections here would be between the academic health centres of the most developed countries and health professionals and students in developing countries.
It may also be helpful to use e-health to augment the healthcare workforce and directly provide the services of doctors, nurses, psychologists, nutritionists and others using telehealth. But the goal is really to build their capacity to the level where it becomes self-sustaining and the most important connections for e-health work become those within a given country or region in the developing world.
What’s appropriate?
e-Health programs must be technologically appropriate. The program should find the most benign technological solution that achieves the desired purpose within the confines of the current social, cultural, environmental and economic conditions of that particular setting. It should also promote self-sufficiency. The characteristics that indicate that something is technologically appropriate are that it is simple to adopt and simple to use, requires very few resources to operate and maintain, and is sustainable and environmentally friendly.
The interactions anticipated in an e-health program must be acceptable locally, and respect local traditions, expectations of the local healthcare system, local beliefs about health and disease and patterns of usage of available healthcare services. Cultural sensitivity training should be provided to anyone working in e-health in another location.
Boundary issues
A former student of mine now based in Karachi called me to ask if I could participate in a teleconference about a possible poisoning of a Canadian national in Karachi. I said yes. But it was not so simple. Higher-ups in my institution at that time were concerned about who would have access to the patient’s records. We have, in Canada, put enormous efforts into protecting the privacy and confidentiality of patients as we create electronic health records (EHRs). We also have very strict rules about who can access a record. As a toxicologist, I am not allowed to access the consult notes in a patient’s EHR, despite the fact that I need to look at all aspects of a person’s work and home life, medications, etc. to assess potential poisoning.
Global telemedicine must contend with the sets of restrictions in place in different settings and recognize that the certification and training of the healthcare professionals involved may be different than those in their own country. Licensure, remuneration, liability issues around professional conduct, clinical standards, accountability for clinical decisions, scope of practice, protection of personal health information, data quality, collection, management — all represent barriers to the global, sometimes even local, provision of e-health services.
Strategy
Global e-health holds promise, but we need to remember the tremendous expense and significant hurdles to e-health in our own countries before proposing it elsewhere. The opportunity costs are not negligible. There have been audited reports in three Canadian provinces and nationally and none of them have come out with a shining recommendation for the EHR or EMR.
Strategy involves clarity about where you want to go, but more importantly why you want to go there. e-Health strategy documents from around the world contain very little explanation as to why a particular direction is viable or appropriate. Only when this is fully understood can it become clear what policy and systems architecture need to be in place to support that direction. We should not get sucked into the technological imperative.
Capacity building is, to my mind, our first priority in global e-health and the countries we want to focus on are largely in Asia, South East Asia, Sub-Saharan Africa and parts of Latin America. We may also, in the interim, be able to use e-health to provide expertise directly, provided we can get around the policy and jurisdictional issues. We currently do this by calling our services second opinion consults, which leaves the local healthcare provider responsible for the care of their patient. This is an entirely viable and appropriate solution, but we know it is a bit of a cover to allow us to creep in under the door and do e-health consultations without having to face jurisdictional issues.
We need to focus now on facilitating interjurisdictional policy coherence, and a number of international organizations have strategy initiatives underway. We are setting the foundation for something that will be in place for a long period of time. It needs thoughtful care, and we need to take the time to do it right the first time.